Article Reviews
★★★★★
I do believe high dose B1 plays a very important role in reducing inflammation through my own research.
My question to you, have you ever come across ‘reactive hypoglycaemia' non diabetic? I read somewhere there is a correlation with Dysbiosis and reactive hypoglycaemia.
Interested in your view, I have been reactive hypoglycaemia for 3 year and have been doing strict Keto, it helps but I do find the diet hard sometimes.
Thanks in advance
Hi Barb,
This condition is new to me so I can't offer any input. This Cleveland Clinic article may be helpful in describing several causes that your doctors may not have checked for yet, such as adrenal insufficiency. The article covers hypoglycemia as well as reactive hypoglycemia and offers some suggestions :
https://my.clevelandclinic.org/health/diseases/11647-hypoglycemia-low-blood-sugar
Art
Article Reviews
★★★★★
Hi Simon,
Thank you for the thoughtful words!
It would be helpful if you had given a bit more information, but I will try to work with what you did give.
Diarrhea is difficult because it is common in diabetics, but it can also be caused by the very common diabetic drug, Metformin, which you may be taking. If Metformin is the cause, you will have to talk to your doctor about using a different drug.
If the diarrhea is caused by the diabetes, it is often caused by peripheral nerve damage which is generally caused by consistently elevated blood glucose which is very damaging to the body in general, so improving insulin sensitivity, decreasing insulin resistance and lowering blood glucose would be the long term fix. One supplement that can help improve the gut microbiome, reduce glucose levels, reduce HbA1c, help with diarrhea, improve colitis and help with peripheral nerve damage is Berberine. You will have to test berberine because in some people it can also cause diarrhea, but in some people it helps alleviate diarrhea.
You mentioned that you have histamine tolerance issues and one supplement that has antihistamine effects, lowers blood glucose levels, works synergistically with Metformin, improves insulin resistance, beneficial for colitis and has a positive impact on the gut microbiome is Quercetin.
You might also give thought to Zinc at 50 mg/day to see if it is helpful in dealing with the diarrhea.
You might also be interested in the following related articles :
https://www.earthclinic.com/cures/six-supplements-for-diabetes-art-solbrig.html
And this one :
https://www.earthclinic.com/cures/insulin-resistance.html
Regarding the H pylori., I'm going to assume that since you were hospitalized for it, they resolved it and retested after you completed the antibiotic regimen.
Keep us posted on how you make out.
Art
Article Reviews
★★★★★
 Jake,
Jake,
Not everyone is sensitive to lectins and lectins seem to cause specific gut issues that can also be seen from causes other than lectins. Some symptoms that some people experience from lectins are the following :
- Neurological symptoms
- Skin Rash
- Hormonal changes
- Gas
- Bloating
- Nausea
- Abdominal cramps
- Painful and or swollen joints
- Allergy like symptoms
- Fatigue
So as you can see, these symptoms can occur in many health conditions, so how do you determine if they are being caused by lectins or something else? I think if I had some of these symptoms and asked my doctor if he thought they were being caused by lectins, he might look at me as though I were crazy and say something like it is likely IBS or some other bowel issue along that line.
To me if you avoid high lectin foods as much as is practical, that makes sense. What is more important to me though, is why do some people have problems with lectins while others do not, even if they are eating foods known to be high in lectins?
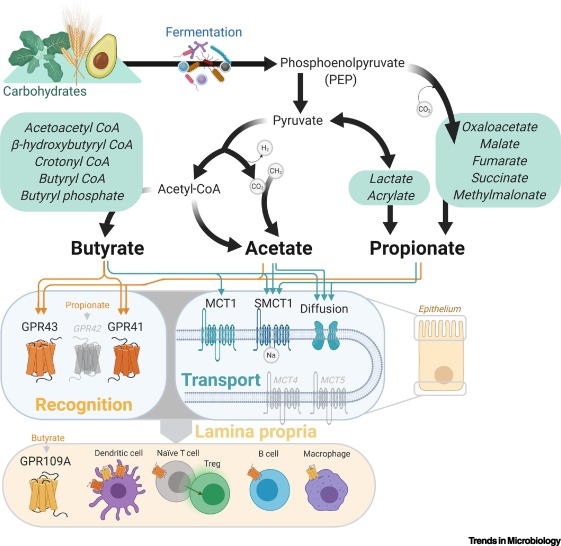
Which brings me to this article that discusses the SCFA, Butyrate and lectins:
Here is a relevant quote from the article :
' We can conclude that KB have a clear suppressive effect on feed intake and growth that is greater in the grower than in the starter phase. Due to the addition of SB in starter and grower feeds, feed intake and growth could be restored up to the level of the control group if KB were only used in the starter phase. When KB were used in the grower phase fifty percent of growth reduction could be compensated by the use of SB. '
So this study shows that the SCFA, butyrate, improved the weight loss caused by kidney beans which are high in lectins.
In this next study it is shown that lectins cause intestinal damage :
Here is a relevant quote :
' Because of their binding properties, lectins can cause nutrient deficiencies, disrupt digestion, and cause severe intestinal damage when consumed in excess by an individual with dysfunctional enzymes. '
The point being that when you look at the damage that lectins can cause to the gut and compare them to the positive gut health effects of SCFAs, a gut microbiome that is well balanced with sufficient SCFAs, SCFA producing gut bacteria, prebiotics and fiber, the SCFAs plus melatonin may nullify, ameliorate or prevent the damage caused by lectins and this could potentially explain why some people seem to handle lectin rich foods with little or no problem while others may not do so well.
These are fine details of research in this area which is not yet fully elucidated, but this would be my general take on lectins. SCFAs in general have the ability to repair the gut mucosal barrier, tight junctions and the gut endothelium and melatonin seems to add synergy in this endeavor to maintain the gut barrier function and gut homeostasis which should compensate for the negative activity of lectins on the gut barrier function when SCFAs and gut melatonin levels are sufficient. That would be my take on lectins given the available studies. This could potentially mitigate the leaky gut that lectins cause. The following article discusses how lectins can cause leaky gut and the associated gastrointestinal distress :
https://health.usnews.com/wellness/food/articles/2017-11-29/the-trouble-with-lectins#:~:text=“For those who eat a, syndrome, system-wide inflammation and
Here is a relevant quote from the article :
' For those who eat a lot of raw, lectin-rich foods – vegetarians or those following a plant-rich diet, for example – the higher lectin intake and the resulting gastrointestinal distress like nausea, diarrhea and bloating can weaken the delicate gut lining, triggering leaky gut syndrome, system-wide inflammation and autoimmune or allergic reactions, ” Lipman says. '
That would be my current opinion on lectins based on the studies I have seen.
Art
Article Reviews
Hi Rachel,
It would help if you can say which vitamins you are referring to, but in my opinion, the exact opposite is closer to accurate. I will give some examples of common vitamins to try and explain what I mean.
Some B vitamins are naturally produced in the gut such as B1, B6 and B12, but in gut dysbiosis, not so much, and this deficiency can contribute to further gut dysbiosis. In the following study it is shown how vitamin B1 plays a critical role in maintaining a healthy gut microbiome and reducing gut inflammation :
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC5613172/
In this next example, you can see how vitamin B2 and vitamin C increased the bacteria Blautia and Roseburria. These two bacteria while in the study did not help much with mucositis caused by methotrexate, are well known as short-chain fatty acid promoting bacteria and this is very beneficial for maintaining gut homeostasis in the bigger health picture!
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC7823339/
In this next study we can look at how vitamin D can affect the gut microbiome in a positive way as well as help maintain the epithelial, but also have a positive effect on autoimmune health issues :
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC6985452/
In this study it is shown that vitamin C, D, and B2 have a positive impact on the human microbiome and barrier function as did vitamin E and vitamin A to a lesser extent:
https://www.tandfonline.com/doi/full/10.1080/19490976.2021.1875774
So I disagree that vitamins are not beneficial for the gut microbiome and as far as vitamin supplementation in relation to fiber and seeds like pistachios, they should be synergistic together, and here is why. Vitamins increase the more healthful bacteria, but these bacteria need food in order to grow and flourish. Fiber is the food of choice for these health promoting bacteria and pistachios are another source of these health promoting bacteria as well as the fiber to feed them.
I hope this clearly explains my thinking on this subject.
Art
Article Reviews
★★★★★
I like you have psoriasis and you're right, psoriasis is a really good way to see how things are working depending on how my psoriasis responds to any vitamin or treatment that I do. I recently have been drinking 1 tsp of borax daily. It has made me feel awesome. It is helping me control my candida and also raise testosterone, and help the parathyroid control calcium production. But, it has made my psoriasis really bad. It has spread all of my scalp and has gotten worse in all the areas that I have psoriasis. Do know of any reason why this is? It is making me feel really good but it made my psoriasis quite a bit worse. Should I discontinue use? Thank you
Hi Jeremiah,
There are multiple ways that people take Borax. You say that you are taking one teaspoon a day, is that one teaspoon of borax powder, or is it a diluted liquid mix? If it is borax powder, then you are taking 4 times more borax than what you should be taking and that dose taken continuously can cause toxicity which could be making your psoriasis worse. Please clarify exactly how much borax and how often you are taking it. Ted only recommended 4 days per week with no borax for the other 3 days of the week. Doing it Ted's way can allow your body enough time to dump any excess borax you may be taking and this can help minimize toxicity issues. If you are taking it seven days each week, that is an even higher dose and of course, that can increase the potential for toxicity even further.
For myself, borax has had zero discernible effect on my psoriasis for good or bad for well over a decade, but it has kept my severe psoriatic arthritis in remission for that same amount of time, which I believe is approaching 14 years. It will probably be helpful to try and first determine if the borax is the cause of your psoriasis exacerbation and the only way I know to determine that is to stop borax at least temporarily to see if your psoriasis starts to improve again. If your dose is high, you should stop anyway to allow your body to dump any excess borax and to also allow your body time to recover from any toxicity issues caused by a borax dose that is too high. When you let me know more about your dose and what else you are using, I can probably tell you more and possibly offer a suggestion or two!
Art
(Houston, TX)
11/25/2021
Hi J,
Do you have parathyroid tumors, because it could be the cause for your elevated calcium. Beware of kidney stones also. Good luck.
Article Reviews
★★★★★
Thank you, Art, for writing this up and sharing.
I've just recently been doing some research myself on increasing resistant starches in the diet to promote a healthy microbiome and heal the gut. Green banana flour appears to be very effective at feeding probiotics and increasing their production of SCFAs. I've even found a couple of recipes that utilize green banana flour. Now after reading your article, I'm inspired to take action! Off to go order some green banana flour and finally start taking the melatonin powder that's been sitting on my counter. I do eat pistachios frequently and will continue to do so! Be blessed!
Hi Madelyn,
Thank you for saying so!
I have tested one type of resistant starch before, potato starch. It is very healthful, but in the potato form, it gave me a ridiculous amount of gas which precluded me from continuing the test beyond one month.
It seems like some of the precursors to Short Chain Fatty Acids (SCFAs) can promote gas as part of the process, beans would be one example, but fortunately not all of them do. Pistachios do not seem to give me gas and I usually eat 3 little cups of them a day. The cup I use is like the ones that they use at restaurants to serve a side of dressing in. My particular cup holds exactly 4 ounces of water when filled to overflowing. I use it as a scoop to dip in the bag of pistachios and I fill it to a rounded top 3 times a day and that is my snack food. That allows me to get a consistent amount of pistachios each day.
Those two FMT studies that I linked to in the article transformed the way I look at treating health issues because while I always knew that maintaining a healthy gut biome was good for your health, I never truly realized how important it is, until I read those studies! Their results were fantastic by any measure. The sad part is that the US is not really pursuing FMT as it should and it is just speculation on my part, but I suspect it is because FMT would essentially take trillions of dollars away from the pharmaceutical industrial complex. There is so much money at risk for them that I can see where they would go to great lengths to see that FMT never really gets off the ground here. Those two studies came out of Asia, which is leading the world in the research into FMT.
That is why I wrote the article because it may be able to replicate FMT with none of the reported risks of FMT and it would be less expensive than FMT.
Good luck and good health on your journey, Madelyn!
Art
(VA)
07/31/2021
Hi Sue,
Thank you for the compliment!
Regarding the pistachios, I am using the ones with the shells. Regarding the shells, these have nutritional value too and in time I am going to experiment with these hulls to see if I can extract some of the nutritional value from them via different methods such as cold water soaking or similarly to the way you make sun tea and then lastly trying to soak them in hot water such as when making regular tea.
My thinking is there has to be a way to take advantage of the nutrients they contain instead of just throwing the hulls away. Thank you for your question, Sue!
Art
(Madison)
07/31/2021
Art, in your article you say that FMT is used for IBS, but I can't find out where in the US that they do this. My gastroenterologist still insists they cannot for IBS-D and I would jump at the chance to do it. I've been on ibs drugs so long that I'm concerned about the impact on my liver, but what's better, Viberzi or tons of immodium? Even on Viberzi, I take 6 - 10 immodium per week. I've done the probiotics for years, using dairy kefir, with no change. Recently did a food sensitivity test and find I'm sensitive to just about all my usual foods, so have changed that. I truly think if my gut was corrected, all my issues with insomnia, reflux, and now thyroid would resolve.
(California)
07/31/2021
GertJr,
The article isn't about FMT so much as trying to replicate what FMT does since use of FMT in the US is fairly scarce. The most advanced studies seem to be coming out of Asia while the US has not completed just 1 study for FMT and PD. The following link may answer some of your questions regarding FMT availability :
https://designershitdocumentary.com/fmt-treatments-therapies/
Good luck and please let us know what you find out!
Art
(Barrie, Canada)
08/15/2021
I suffered with IBS for years. Solved with energy healing focused on Vagus nerve. Try imagine lighting bolts shooting through the middle of your body, head to toes. Very well known energy healer Adam McLeod held the group therapy for fibromyalgia sufferers. My pains were not gone, but my IBS and tiredness were gone. you can buy his books explaining the procedure.
(CA)
11/07/2021
Gertjr, Call Dr. Mark Rosenberg in Boca Raton, FL to ask about FMT for your issue. He does the procedure but not sure for what diseases.
(VA)
07/31/2021
Thank you, Art, very interesting!
Article Reviews
★★★★★
It would be helpful to know how much B-12, how many pistachios, etc, you are taking each day. There are plenty of us out there who want to experiment right along with you! I've been gut sick for decades.
Thanks,
Clare
Hi Clare,
I am not a doctor so I can only say what I am taking.
The minimum amount of vitamin B1 that I personally take is 200 mg day and I go as high as 600 mg, but mainly average 400 mg/day. I usually take it in two divided doses, one at or before breakfast and the other dose at or before lunch. I try to avoid taking B-1 later than 2:00 pm because in some people it can cause sleep issues, so I use 2:00 pm as my limit. I do take one vitamin B-50 a day to try and keep the B vitamins in balance.
Pistachios are now my main snack food and I use a little cup such as they use at restaurants for sides like salad dressing. The one I use holds exactly 4 ounces of water when filled to the very top. I scoop this into my big bag of pistachios and fill to a rounded top. I eat 2 or three of these small cups a day.
Melatonin as I have mentioned previously, I take a minimum of 106 mg per night and have done so for many months now, but the idea of rebalancing the gut microbiota is to increase Short Chain Fatty Acids and increasing those will increase gut melatonin production so that supplementing melatonin should not be needed in time. I am mainly supplementing melatonin right now, to test whether it can speed the process up a bit. I expect, that similarly to FMT, it may take 3 months to see good benefit. Melatonin produced in the gut does not cause the "melatonin hangover " that some people experience from supplementing melatonin.
I have not as yet started intermittent fasting and may not need to because my results are fairly good so far.
I am eating oranges and will begin including apples to increase fiber. Apples have pectin which is helpful toward increasing SCFAs. I am trying to keep it as simple as possible and I hope this answers your questions.
Art
Article Reviews
★★★★★
(Idaho)
07/30/2021
★★★★★
Thanks for posting this! I wouldn't have seen the article otherwise. Smiles and thank you!
Article Reviews
★★★★★
Thank you for such an informative article on the gut microbiome (our second brain, they say).
I'm also very impressed that you are experimenting on yourself and sharing the results!
As you know, I've used your borax remedies with great success and I now take melatonin on a regular basis (still at the low-dose stage, though).
Excellent work, Art.
Cheers,
Tessa
Thank you for saying so, Tessa!
If we can get the SCFAs increased, supplementing melatonin should not even be needed anymore as the SCFAs should build it up in the gut to healthful levels which in turn should also apply its positive effects to the gut and the brain via the gut/brain axis!
Art
(France)
07/30/2021
I can recommend the web site culturedfoodlife.com, They have a wealth of information for cultured food and pro and prebiotics.
BPC-157
★★★★★
(ON)
01/20/2024
(Idaho)
04/08/2024
Butyrate
★★★★★
https://www.ihcanconferences.co.uk/butyrates-impact-on-the-microbiome-and-neuro-function-ihcan-conferences-webinar/
pdf of presentation also available. https://www.ihcanconferences.co.uk/downloads/2021/webinars/butyratebodybiowebinarslides.pdf
(CA)
11/09/2021
Along with adding more anti-cancer foods for gut biome health I also take a butyrate supplement. Testing on the cancer showed butyrate as very high on the list I needed to address.
Frances,
This is a topic that I am interested in.
Butyrate is one of the three predominant short chain fatty acids (SCFAs). The other two predominant SCFAs are acetate and propionate. We can increase SCFAs by eating the right types of soluble fermentable fiber which feeds the healthy SCFA producing bacteria in our gut. Prebiotics also increase SCFAs. Increasing SCFAs in this way increase all 3 predominant SCFAs which include butyrate.
Butyrate interacts with the epithelial cells to increase melatonin production in the gut while propionate and acetate increase melatonin receptors in the gut. In turn, melatonin increases SCFA production in the gut in a pro health cycle that is stimulated by increased fiber intake. Together butyrate and melatonin both help repair the gut mucosal barrier which helps to prevent gut permeability (aka leaky gut) and beyond the mucosal barrier they also strengthen the epithelial barrier to further repair gut permeability. This is very important for maintaining the best health.
The downside is that in some disease states, the SCFA producing bacteria can be very low, in which case SCFA production may be minimal and this can allow the mucosal barrier to become perturbed which allows gut permeability to increase allowing bacteria to escape the colon into the general circulation which causes an inflammatory response by the body to attack these bacteria that the body sees as invaders. This inflammatory response results in significant collateral damage as well as further increased inflammation and oxidative stress which is all bad for our health.
Melatonin and the SCFAs have antiinflammatory and antioxidative effects in the gut aside from their ability to improve gut permeability which is very good for improved health. Unfortunately, SCFAs decline with age and decreased SCFA production in the gut results in decreased melatonin and melatonin receptors in the gut and all of this results in ill health and disease. Exercise increases SCFA production as does fasting.
A few vitamins have shown some ability to increase SCFAs. Fasting can also increase SCFAs. Pistachios can increase SCFAs and also contain significant amounts of fiber. Prebiotics can increase SCFAs.
Art
(Barrie, canada)
11/11/2021
I read it just yesterday: connecting Byturate levels with ME/CFS!
https://www.healthrising.org/blog/2021/11/10/bacteria-fatigue-chronic-fatigue-syndrome/
(U.K.)
11/12/2021
Grass fed butter is a great source of butyric acid.
(CA)
11/12/2021
Yes, truth. We only use grass fed butter.
(Sacramento, CA)
12/30/2021
(CA)
12/30/2021
Bobbi,
A few things that are useful to fight H. Pylori are: Mastic Gum Oil of Oregano, Monolaurin Grapefruit Seed Extract (GSE) Colloidal Silver Nanoparticles (AgNPs) GSE and AgNPs are both biofilm busters which will be important in a long standing overgrowth Probiotics: L . Acidophilus L. Rhamnosus L. Plantarum
Art
(Daytona, FL)
12/05/2024
I want to ensure that people know that the butyrate supplements currently on the market are dangerous. They added hydroxides to up the pH, and instead of bringing up to neutral, which wouldn't have been needed to start with, they increase it to a pH of 9+. They likely state that this is to "combat the acidity" or something, all the while your stomach naturally has a very low pH as is needed. You DONT want to increase your stomach pH. If you get butyrate supplements, I'd recommend either adding ACV to it before hand to neutralize it, or add the contents to an acidic soup.
Digestive Enzymes
★★★★★
Peter,
I think digestive enzymes can be useful in some instances and I think it is more useful to try and correct the underlying gut issue, but this can be hard and time consuming to determine what the underlying problem is and then try and correct that.
As an example of a simple use of digestive enzymes, a friend had a dairy intolerance issue where ice cream gave him an overabundance of gas which he was able to avoid by taking the Now Brand Super Enzymes before eating ice cream.
In another friend who had the feeling of indigestion with the urge to defecate everytime he ate, those same digestive enzymes were completely ineffective.
Digestive enzymes can also help some people with gluten intolerance. There are many reasons for digestive issues and digestive enzymes will help with some, but they can make others worse.
Art
(New Zealand)
01/04/2022
Fermented Foods for High Blood Pressure
★★★★★

I have a story of extreme High Blood Pressure (over 200) and how I corrected it within 15 days, returning it to a good healthy range of 117/73. If you find yourself in a situation where you suddenly have high blood pressure where you had never before I suggest you look for outside influences that might have caused the situation. Let me tell you my story and let you draw your own conclusions.
I am a 53 year old healthy male. I do not take any medications and am proactive with my health. I believe that nutrition (from whole food sources not vitamins from bottles which a very high number on the market are of a synthetic nature and just don't work) is the key to good health. When a problem occurs with my health the first thing I do is sign onto Earthclinic and look for solutions based on a whole foods approach. By whole foods I mean as close to grown from the earth as possible. This means herbs, roots, food based vitamins/minerals, spices, vegetables, wheatgrass, (and so many more) and products made from these).
So last year I had some dental problems which necessitated numerous rounds of antibiotics - 3 rounds of amoxicillin and one round of penicillin over the course of a year. I had a recurring infection in a front tooth. I did not want a root canal instead I opted for an implant and was using the year to save up for the procedure. I foolishly thought that antibiotics could handle any flare ups until I could get the procedure done.
When I went into the specialist to get the implant he checked my blood pressure as he would have to put me under to do the implant. At that moment he bluntly told me that he would not do the implant and that I needed to see my doctor immediately. If I did not, I could suffer a heart attack or stroke at any moment. He went on to say my blood pressure was over 200, well in the danger zone. He refused to do the implant until I was on medication and my blood pressure was in the normal range.
I left the dentist office in shock. I had never had high blood pressure. As soon as I got home I got on Earthclinic looking for help. I found a post on how one cup of Kefir (fermented yogurt drink) every day could help lower your high blood pressure and that a compromised gut biome from taking too many antibiotics could cause a wide range of health issues one being high blood pressure.
By gut biome I mean the healthy microbes and bacteria in your gut that helps you break down food and assimilate it for the body's health. At this point I was willing to try anything. I did not want to go on any medication. I decided I would do a test to see if kefir and fermented food in general would work in lowering my blood pressure. I purchased an inexpensive blood pressure monitoring cuff from Amazon for around $25 and headed to Walmart to purchase some kefir (in the refrigerated yogurt section) and a health food market to get some fermented Sauerkraut and fermented pickles (because they are fermented - I.e. live foods - fermented sauerkraut and pickles must be refrigerated. You'll find them in the refrigerator section of a health store where they sell pickles).
I figured the more fermented food the better. I would drink one cup of kefir in the morning, eat 1/2 cup sauerkraut at lunch and dinner (twice a day), eat 1-2 pickles for snacks, and drink one ounce of the fermented sauerkraut and/or fermented pickle juice a day (fermented juice is loaded with probiotics). One word about sauerkraut, I am not a fan of many of the brands on the market except one - I'm not sure I can say the name on earthclinic but it is one word, begins with B, and is seven letters. I found this brand to be very tasty. They also make the fermented pickles, just as tasty).
The experiment was simple. I would consume the fermented foods in the proscribed manner mentioned above and check my blood pressure every morning before any food or coffee. I didn't notice any change in my blood pressure until around the 5th day. That day it dropped two points. and from there it rapidly dropped. After 15 days my blood pressure was 117/72 in the healthy good range.
I continued with the routine for another two weeks then weaned myself off the kefir. I still eat one 1/2 cup of sauerkraut or one pickle or drink one ounce of fermented juice a day as a good health routine. It has been a year since doing this and I feel so much better. I find I sleep better, have less stress, less depression, and a higher overall sense of well-being. I just had a full doctor's checkup with full blood work and everything came back excellent.
The doctor gave me a clean bill of health. So get out there and try fermented foods - they do work.
(Kansas City)
08/07/2021
★★★★★
I too drink a shot of sauerkraut juice every night I also use Keifer in the mornings. I do not eat any wheat at all in anything; I have never felt better. My veggies consist of Bibb lettuce, Napa cabbage, onions, for dressing Apple cider vinegar
(TX)
08/07/2021
I am glad you shared your story. My BP (after anesthesia at the dentist's office three years ago) has gone up to 190/107 and has never come back to normal, which scared me because I consider myself generally healthy eating fruit, some fish and cheese. I also take food supplements. Nothing has worked so far from bio-magnets, Reiki, massage or diet. I am trying fasting now as a last resort. Thank you for sharing. I will do the kefir tomorrow and then see if I get some sauerkraut juice as well. Blessings!
(somewhere, europe)
08/08/2021
Yasmin, you might want to add veggies to your diet and water as per Dr. Batman..
(AZ)
08/07/2021
Make your own kraut. American Indian style (Eastern) is cut up the cabbage, pack in a large jar, and if needed, add water. Press it down in the jar with something. No salt! Do not tighten the cap because it might crack the jar. Put the jar in a bowl, because without salt and in the heat, it about boils in the jar. This is called summer kraut and if the heat is 80+F, you'll have it fermented in a week to 10 days.
(Orl Fl)
08/07/2021
(UK)
08/08/2021
Well done a hero for the battle against disease!!
Recently I have had tooth pains and associated neuralgia in the head ie various types of headaches engendered by the state of my bad teeth. I have no need for anti-biotics, I just do:
Oil pulling three times a day for a week then twice a day. Also used a strong sea salt solution, swish that around the mouth for about 3 minutes three times a day if you can. Complete cure in 3 days.
Oil pulling can be various oils such as coconut oil then after a couple of days run out of coconut oil so used virgin olive oil, mixed about 20% neem oil in to make it even more powerful. take about one or 2 teaspoons and swish around mouth for at least 10 minutes then spit out.
(Michigan)
08/08/2021
I too, was going to have a procedure to remove a tooth due to infection in the dental office and had high blood pressure. My dentist yelled at me and told me to take a pill. I feel she was more upset about losing a sale than my well being. She let me leave without antibiotics. I am excited to try the kefir and sourkraut. Thank you for the info!
(TN)
08/08/2021
It is ok to mention the brand. We have the right to choose which is best. thanks.
EC: Yes, if he wants to post it, no problem.
(Idaho)
08/09/2021
I believe the brand he was referring to is BUBBIES. They make naturally fermented, live culture sauerkraut and pickles. Yum!
(Indiana)
08/09/2021
FYI, Bubbies actually kills off a portion of the beneficial bacteria before shipping to give their products a longer shelf life (I believe this is on their website). It's best (and more rewarding) to ferment your own products. There are many books and videos on how to do it.
(Alexandria, VA)
11/05/2021
(MPLS, MN)
12/17/2022
(Australia)
05/10/2023
Make your own fermented foods, its not hard nor does it take a lot of time and its cheaper and better for you. Use organic ingredients. I've made sauerkraut, kefir, kombucha, pickles.. Youtube and health conscious sites have tutorials etc
FMT for Diabetes Type I
★★★★★

I also said I would update as I found new info about gut microbiome manipulation. Many of you may be aware of how serious a disease Diabetes Type 1 is and how difficult it is to treat with treatments oftentimes not being very effective. I came across a human study yesterday that illustrates just how powerful the effects that gut microbiome manipulation can be on human health.
This newer Randomised Controlled Trial (RCT) (2021) used FMT as the means to manipulate the gut microbiome of relatively newly diagnosed (less than 6 weeks) Type 1 Diabetic patients.
This is the title of the study :
Faecal microbiota transplantation halts progression of human new-onset type 1 diabetes in a randomised controlled trial
Here is a link to the full study itself:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7788262/
This study and other recent gut microbiome studies start to give us clues of how broad and how powerful the health effects of microbiota manipulation are in humans!
Art
Gut Microbiome and Autism
★★★★★
MY son is autistic. I heard that a bad gut is one of the big reasons for autism and the behaviour of autistic people. By curing a bad gut the behaviour pattern changes to good. Is there any chance of bringing the communicative skills can be improved. Any other suggestions? Please
Hello natarajan,
All we really have to use as a guide is results that have been obtained using the Fecal Microbiome Transplants and benefits have been shown using FMT for Autism. Here is a link to an article that discusses FMT results in patients with Autism that was done at Arizona State University (ASU) :
https://www.sciencedaily.com/releases/2019/04/190409093725.htm
I would highly recommend contacting the research team at ASU to find out if they have done further studies or if they think that modifying the diet might be helpful. The following link may also be helpful in your search:
https://designershitdocumentary.com/fmt-treatments-therapies/
Please update us on your findings.
Art
(Israel)
08/08/2021
Look into information about the GAPS Diet. It is about the microbiome, the gut and how it affects the mind and the development of the child.
(Orlando, FL)
08/09/2021
By all means look into the GAPS diet. www.gapsdiet.com
(Bigfork, MN)
01/21/2022
★★★★★
Yes, we had our son tested for food sensitivities, removed those foods to stop the inflammation in the gut. Then you can start rebuilding the normal flora in the gut. Within 3 weeks we saw significant improvement in our son's behavior, communication, and he seemed to be aware of his surrounding for the first time. We made the change when he was 7, he is now 11. He is behind his peers in school but is making steady progress... if you make these changes you will not regret them.
Best of luck.