-
Health Ailments
- All Conditions A-Z
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's | Dementia
- Borax
- Cancer
- Chronic Pain
- Colds and Flu
- COPD
- Coronavirus
- Crohn's Disease
- Depression
- Fibromyalgia
- Erectile Dysfunction
- Heart Disease
- High Cholesterol
- IBS
- IPF
- Menopause
- Osteoarthritis
- Psoriasis
- Sinus Infections
- Type II Diabetes
Alzheimer's Disease: The Gut-Brain and Microbiome Connection
Alzheimer's Disease (AD) is the most prevalent form of dementia and tops the list of neurodegenerative diseases, followed closely by Parkinson's. As an age-related disease, the risk of developing AD increases with age. Unfortunately, the current prescription medications for AD offer only minimal effectiveness. Even for those few who do benefit, the positive effects are often fleeting.
The latest potential AD medication, Donanemab, has shown promise in slowing disease progression more effectively than a placebo. However, its phase 3 trial revealed concerning side effects, including brain swelling and death—three of the four patient deaths were concluded to be drug-related. While it might offer a slower progression of the disease, its risks highlight the pressing need for alternative methods to combat AD's advance.
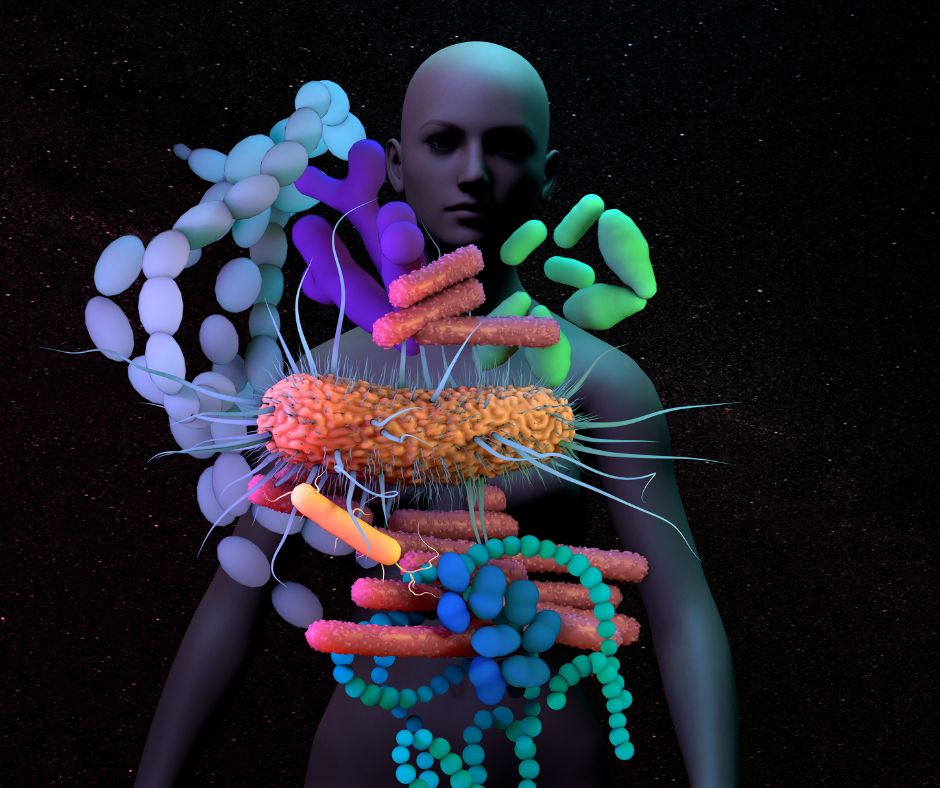
Alzheimer's Disease and Gut Microbiome
I have been reading many studies related to AD and saw studies suggesting that the status of the Gut Microbiome (GMB), or the microbes that live in your intestines, can affect the disease in good or bad ways. There is research available suggesting that the state of your GMB is intimately involved in the progression of Alzheimer's Disease (AD). It is thought that gut dysbiosis, which means that there is an imbalance of microorganisms in the intestines that favors pathogenic bacteria, is seen in people with AD.
The following 2023 review of this aspect of AD is quite informative in this respect:
https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-023-00595-7
Here are some very relevant quotes from the review that tend to support the idea that the state of the GMB is very important in relation to AD status:
' Amyloid beta oligomers and plaques, tau aggregates, and neuroinflammation play a critical role in neurodegeneration and impact clinical AD progression. The upstream modulators of these pathological features have not been fully clarified, but recent evidence indicates that the gut microbiome (GMB) may have an influence on these features and therefore may influence AD progression in human patients. In this review, we summarize studies that have identified alterations in the GMB that correlate with pathophysiology in AD patients and AD mouse models. Additionally, we discuss findings with GMB manipulations in AD models and potential GMB-targeted therapeutics for AD. '
' Two initial studies in 2017 showed that amyloid-positive individuals/AD patients have an altered GMB composition compared to individuals without amyloid/AD. '
' Here, a decrease in GMB bacterial diversity was observed in AD patients, as well as a decrease in Firmicutes and Bifidobacterium and increased levels of Bacteroidetes compared with HC. Since these initial studies, two other studies from groups in China also found alterations in GMB composition between AD patients and HC. Zhuang et al. (N = 86, 43 AD, 43 healthy controls) found a decrease in Bacteroidetes and an increase in Actinobacteria in AD patients compared with HCs. Liu et al. (N = 97 total, 33 AD, 32 MCI, 32 healthy controls) found a reduction in Firmicutes and an increase in Proteobacteria in AD patients compared with controls. Taken together, the results from these studies suggest that GMB composition is altered in AD patients and that GMB changes may have an influence on the progression of AD. '
The review went a couple of steps further by suggesting that manipulating the GMB through various means, such as Fecal Microbiota Transplantation (FMT), might positively restrain or alter the disease process. Here is a relevant quote:
' In AD, a pair of studies were published recently demonstrating the effectiveness of FMT in reducing pathology in AD mouse models . Sun et al. (2019) showed that administering FMT from WT mice into 6-month APP/PS1 mice for 4 weeks resulted in a reduction in Aβ, tau hyperphosphorylation, increased levels of synaptic proteins, and decreased cyclooxygenase-2 (cox-2) and CD11b + microglia . Kim et al. (2019) corroborated these findings in the ADLPAPT mouse model of AD by showing that treating ADLPAPT mice from 2 months of age with WT FMT until 6 months of age resulted in a reduction in Aβ, tau phosphorylation, Iba1 + microglia, GFAP + astrocytes, Ly6Chigh monocytes, and better performance in contextual fear conditioning and Y maze. '
To add a human context to the above reports of FMT treatment in an AD animal model, the following link takes you to a case report of an 82-year-old man who was diagnosed with Clostridium difficile (C. diff) that standard treatment had failed to help (qualifying him for FMT), he also had MRSA resistant pneumonia and AD with five years of disease progression and memory loss to a point where his AD meds were no longer sufficient to offer much help. His wife reported that he was socially withdrawing and was suffering cognitive decline.
https://journals.sagepub.com/doi/full/10.1177/0300060520925930
This case report is interesting because the FMT did significantly more than help the C. diff as described here:
' At the follow-up visit 2 months post-FMT, the patient’s wife reported improvements in the patient’s mental acuity and affect. The MMSE was re-administered by the gastroenterologist (and subsequently by the neurologist) and the patient scored 26, indicating normal cognition. Four months post-FMT, the patient reported continued improvement in memory, with no progression in symptoms. The patient now remembered his daughter’s birthday, which he had not been able to recall previously, and was able to correct the physician’s recollections of his symptoms. Six months post-FMT, the patient reported a marked improvement in mood, was more interactive, and showed more expressive affect. Readministration of the MMSE revealed that the patient’s score had further increased to 29. '
The study came to the following conclusion:
' To our knowledge, this is the first report of a case of rapid reversal of AD symptoms in a patient following FMT for recurrent CDI. Improvements in AD symptoms occurred as early as 2 months post-FMT and continued to the 6-month follow-up visit (the date of the last follow-up), with no noted reversion of symptoms. The resolution of symptoms occurred in a stepwise manner: first, there was increased mental acuity and improved affect observed at 2 months post-FMT, and this was followed by marked improvements in memory and mood by 4 and 6 months post-FMT, which were accompanied by more expressive affect. These findings paralleled improvements in the patient’s MMSE scores, which increased to within the range of normal cognition by 2 months post-FMT. Eradication of CDI was also confirmed at the 2-month follow-up visit, via the resolution of symptoms and a negative stool test. '
In this next case report from August 2021, a 90-year-old woman was diagnosed with Clostridia difficile (C. diff), which qualified her for FMT. She also has Diabetes Mellitus Type 2(T2DM), hypertension, chronic kidney disease (CKD), diarrhea, fever and a 5 year cognitive and memory decline due to AD.
https://www.tandfonline.com/doi/full/10.1080/03007995.2021.1957807
Here is a relevant quote from the case report:
' One month before admission, she underwent cognitive function evaluations (Mini-Mental State Examination [MMSE], Montreal Cognitive Assessment [MoCA], and Clinical Dementia Rating [CDR] assessment) for ∼30 min by the neurologist (Supplemental Table 1). The cognitive tests revealed significant impairments in the areas of short-term memory, semantic skills, attention, non-verbal learning, and response inhibition (MMSE 15, MoCA 11, CDR 1; Table 2). '
Here is another important quote from the case report :
' She was diagnosed with severe CDI, and after failed treatment with several antibiotics and aggravation of symptoms determined by a positive CDI stool test, she underwent FMT following FMT indicationCitation5. She did not present with any delirium due to CDI or medication as determined by a delirium assessment scale (4 A’s test [4AT] score 1). '
I'm just going to go ahead and say what many people are probably thinking, a 90-year-old person with this many health conditions should be making funeral arrangements instead of trying FMT. In fact, such a plan to make funeral arrangements would have been a mistake of major proportion based on the following results! Also, the speed with which FMT seems to work is impressive for a disease that takes many years to manifest.
1. Following the first FMT, her severe gastrointestinal symptoms improved, and a stool test for CDI was negative. One month after the first FMT, her cognitive functions slightly improved (MMSE 18, MoCA 12, CDR 1; Table 2, Figure 1).
2. Three months after the first FMT, the patient experienced watery diarrhea, fever (38.0 °C), continuous abdominal pain, and progressively worsening conditions. However, she did well in blood sugar test control for DM treatment (HbA1c 6.1), and her vital signs were stable (140/82 [mmHg]–88 [beat/min]–20 [breath/min]). She was diagnosed with a recurrent severe CDI for a positive CDI stool test unsuccessfully treated with antibiotics. She underwent a second FMT with the same modalities as the first transplantation Citation5.
3. Her MMSE, MoCA, and CDR scores before the second FMT procedure were 20, 16, and 0.5, respectively, an improvement over her results immediately after the first FMT. In addition, similar to the previous admission, during the second admission also, she did not present with delirium (4AT score 1). Her general physical condition did not affect her cognitive functions ( Table 3). One week after the second FMT, her severe gastrointestinal discomfort improved with negative CDI stool results. Her scores were stable (MMSE 20, MoCA 17, and CDR 0.5), and she reported a marked improvement in mood (GDS 17) and daily living activities and showed more expressive affection (Figure 1).
These results allowed the research team to arrive at the following conclusion:
' In conclusion, our case provides evidence of the benefit of FMT in patients with cognitive decline and the efficacy of FMT. Furthermore, it suggests an association between the gut microbiome and cognitive function and its potential as a therapy for AD. '
I find it very interesting that FMT appears to show results in as little as one month in many studies. I have previously written extensively about FMT and the 85 diseases that it has been tested for while answering many questions that people typically have about its use. Here is a link to that article:
https://www.earthclinic.com/remedies/fecal-microbiota-transplantation-exploration.html
So these case reports are quite interesting and suggest that altering the gut microbiome correctly can significantly improve AD symptoms and disease markers. To add further confirmation to this idea that positively altering the gut microbiome can help alleviate AD symptoms.
The following study also tried to manipulate the gut microbiome via a different method in a group of AD participants via four common and inexpensive probiotics that were delivered in a daily glass of 7 ounces (200 ml)of milk at high doses, as discussed in the following human study:
https://neurosciencenews.com/alzheimers-probiotics-5481/
Here are some relevant quotes from the study :
' For the first time, scientists have shown that probiotics — beneficial live bacteria and yeasts taken as dietary supplements — can improve human cognitive function. In a new clinical trial, scientists show that a daily dose of probiotic Lactobacillus and Bifidobacterium bacteria taken over a period of just 12 weeks is enough to yield a moderate but significant improvement in the score of elderly Alzheimer’s patients on the Mini-Mental State Examination (MMSE) scale, a standard measure of cognitive impairment. '
' Here, the researchers from Kashan University of Medical Sciences, Kashan, and Islamic Azad University, Tehran, Iran, present results from a randomized, double-blind, controlled clinical trial on a total of 52 women and men with Alzheimer’s between 60 and 95 years of age. Half of the patients daily received 200 ml milk enriched with four probiotic bacteria Lactobacillus acidophilus, L. casei, L. fermentum, and Bifidobacterium bifidum (approximately 400 billion bacteria per species), while the other half received untreated milk. '
The study concluded the following:
' The current study demonstrated that the probiotic administration for 12 weeks has favorable effects on MMSE score, MDA, hs-CRP, markers of insulin metabolism and triglycerides levels of the AD patients; however, the changes in other biomarkers of oxidative stress and inflammation, FPG and other lipid profiles are negligible. '
Since having more studies to corroborate the results of this 2016 study would be useful, I found a 2023 meta-analysis of multiple randomized controlled trials (RCTs) using probiotics for AD here :
https://pubmed.ncbi.nlm.nih.gov/36629438/
Here is a relevant quote from the meta-analysis that tends to confirm the findings from the 2016 study showing that the proper manipulation of the gut microbiome via the use of probiotics has a significant positive effect on cognition and AD:
' According to this meta-analysis, probiotic supplementation had a highly significant effect on cognitive function in people with cognitive impairment or Alzheimer's disease. For people without cognitive impairment, probiotic supplementation may be ineffective. '
Given the conclusion of this meta-analysis seven years and many studies after the 2016 study in conjunction with the FMT case reports, it is clear to me that gut microbiome manipulation via various means is significantly more effective than any of the current drugs that are prescribed for people with AD and have significantly better safety profiles also.
This information begs the question of why the scientific community is spending scarce research funding pursuing questionable targets when it is clear that the science can obtain significantly better results through gut microbiome manipulation via relatively inexpensive means such as probiotics, FMT, and other techniques. Just imagine being able to treat the number one neurodegenerative disease in the world with a well-designed Probiotic.
Previously I wrote about supplements that can help with memory loss here:
https://www.earthclinic.com/cures/art-solbrig-protocol-for-memory-loss.html
Interestingly, these five supplements also positively impact the gut microbiome. Perhaps just a coincidence, but I tend to think it is not a coincidence at all.
Conclusion
With each passing year and each passing study into AD, it is becoming clearer and clearer that the state of the gut microbiome (GMB) is a major player when it comes to AD. Gut microbiome dysbiosis is a given when it comes to AD, and more and more studies are showing that AD can be positively affected by manipulating the gut microbiome away from dysbiosis toward health-promoting bacteria. Fecal Microbiota Transplantation (FMT) and probiotics are just two effective ways of doing this, with FMT seeming to be the more efficacious of the two methods, and both methods are relatively inexpensive compared to what it costs to maintain a person with AD once they are no longer able to care for themself.
GMB manipulation has been shown to be safe and effective with very limited side effects. The studies already show that it works, but science continues to delve into other target areas of AD that are very likely downstream and not as effective as correcting gut dysbiosis to significantly improve AD symptoms and make life livable again for people with AD well beyond what the current prescription meds can do.
Art
Related Links:
Art Solbrig's Memory Loss Protocol
FMT: Trailblazing Gut Health & Microbiome Restoration
Natural Remedies to Support Brain Health and Reduce Alzheimer’s Risk
Top Natural Remedies for Memory Loss
Alzheimer's - Microbiome Link
Natural Remedies
You must be logged in to this post! Please sign in:


